I truly never thought I’d have surgery again. My last surgery was a major de-bulk after my metastatic pheochromocytoma diagnosis.
But that was before getting diagnosed with a whole other cancer… catch up here on the whole thyroid saga
After the agonizing drawn out process of diagnosis, things moved QUICK.
Normally, you’d have to wait until after surgery in order to even know what variant the cancer is. Pathology tests less than 30 genes, but if there’s something we know around here: knowledge is power.



Thanks to a whole lot of kind people, I was able to get the thyroseq V3. A molecuar sequence test that could tell us a whole lot more before surgery. The results granted me the knowledge of knowing I have a rare variant of papillary thyroid carcinoma (PTC) – called ‘diffuse sclerosing’ and a genetic mutation called RET PTC1. All of which would impact the future of how we treat it, and the current timing of how we intervene.
Of course, rare. Very on brand for me 🦓
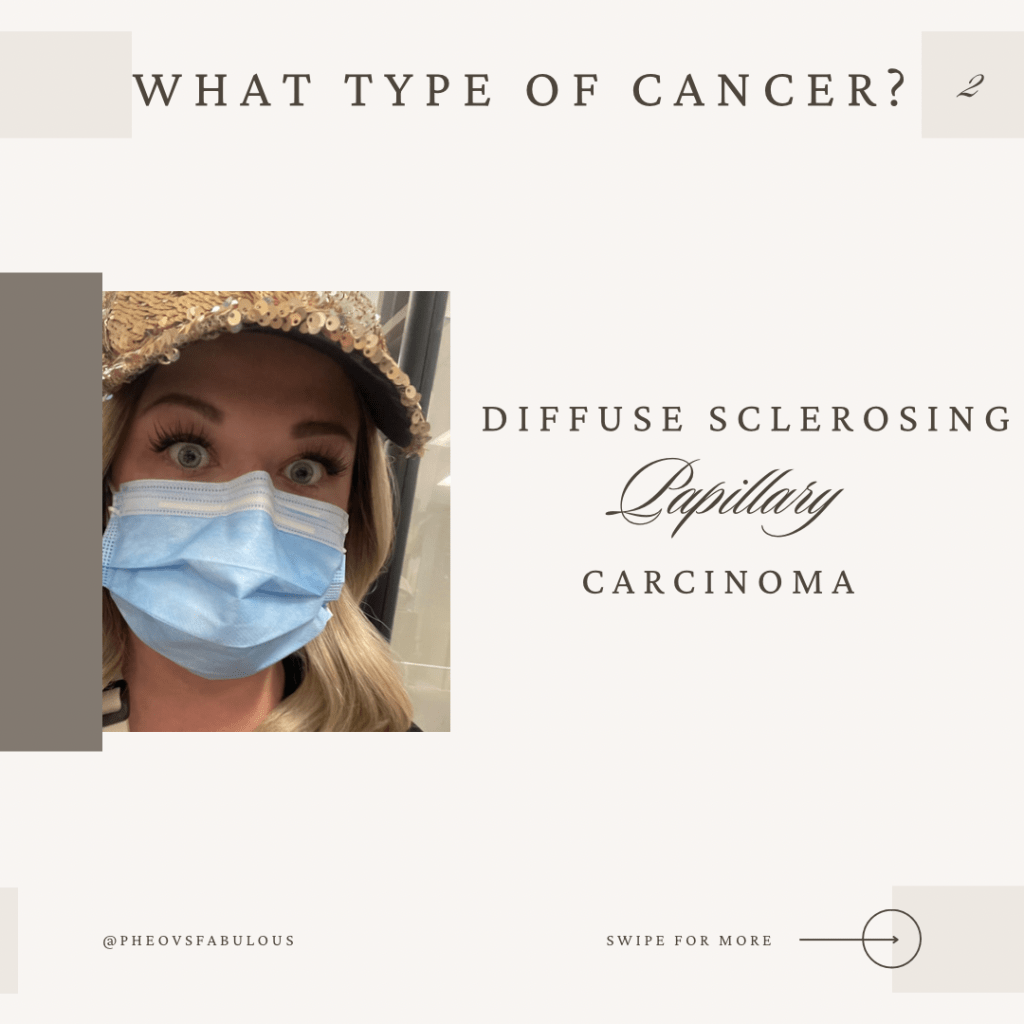



Knowing that this variant is more aggressive than the more common PTC, we had to act quickly. Well, hearing the word metastatic made ME act quickly regardless. I wasn’t willing to wait more than 6 weeks for surgery from the time I heard the word cancer.
I may have had a heck of a time getting a diagnosis… but man my entire team SHOWED UP for me once I did.
Doctors texting one another, my name being brought up constantly, reassuring me the wheel is turning, the planning, careful attention to my stress levels, pressure for OR time, pushing for me when my surgery date was pushed. It was truly amazing, and these measures don’t go unnoticed.
I remember my endo personally enlisting the help of a thyroid cancer specialist to expedite the diagnosis and do the molecular testing in the private clinic. Within an hour we were seen.
When Dr.P called me to confirm I had thyroid cancer, I was trying to stay calm while trying to foresee every potential objection. He stopped me by saying “Let me be your advocate. You can stop advocating now, just focus on getting through surgery”

I think we both knew I’d never be able to stop, but… it was a really big relief to hear that. That meant I could focus my energy into my biggest self advocacy project yet. The Miranda Protocol
Yes, I created a whole medical protocol that would be required to keep me safe and stable throughout the surgery. I’ve been told I’m too complex, too rare, too complicated. this would act as my personal instruction manual to deconstruct those objections. It would leave no room for the avoidable error, and would use previous experience to unravel the complex care needed.
Truthfully, I had no idea how it’d be received. I was stressed. I was nervous. I was intimidated thinking about making the pitch to my doctors. Who do I think I am?
Being denied surgery made me feel I have to tread carefully, not wanting to seem too complex or that I could be denied this privilege at any moment. Not wanting to seem too sick, too needy, too much. I made myself smaller to receive the care I needed, and I knew that was going to hurt me even more if I continued.
I’m pheo vs fabulous. I’m Miranda, and I am so much more than any diagnosis. I am an expert advocate. I have helped so many people to find the confidence to properly advocate for themselves.
What would I be saying to someone who’s in the same situation?
It’s time to take your power back.
Just for reference, my timeline was tight. I was diagnosed on December 8th, and the surgery was to be within 6 weeks. We had no date and very little available OR time. We had to orchestrate a fundraiser campaign in just one week for the thyroseq V3. We had to make arrangements for an extended stay in another city to be close to the hospital for a month. We had to figure out care for our blind senior fur baby, William. I had to write my own medical protocol from scratch. We were also searching for a place to live closer to the hospital. Knowing we couldn’t sustain this chaos.
I had to stay calm and stress free (lol) since my body was on fire with Graves’ disease and my mast cells were not having it. I was worried about how that would impact the cancer’s growth. I was researching how they’re all linked together. I was restless and my legs wouldn’t calm down making me scream into my carebears at 4am. Serge aka doctor cupcakes finding ways to soothe me, late night walks, CBD rubs, baths, moral support. (Shoutout to him for listening to my never ending rants to try and facilitate all this) We were travelling multiple times a week to get labs and each day would turn into a marathon of unplanned appts. Meanwhile I was wondering if my careful efforts to stabilize the metastatic pheos would become unhinged. I was trying to find ways to think clearly while the thyroid hormones clouding my judgement. I was learning which symptoms were which so I could appropriately respond to each storm. I was severely overwhelmed to my core but just had to find a way to keep going. I had to find a way to believe it would all be OK

I felt like a human pin cushion, my neck getting a lot of attention and a lot of needles. Surprise biopsy after biopsy, I was feeling a bit bruised and battered 😅 but the show must go on!

Christmas came and went, that was my marker that I needed to get really serious. The Miranda protocol had to be finished yesterday, and signed off by my doctors. I had to sit down with each one and ensure it was done with the same conviction I had. It was all in my brain, I just needed to sit down and formulate all of the information. It had to be clean and cohesive. It had to be usable and extensively reviewed.
I started by using my medical resume format as the inspiration. Starting with the basics, what do they need to know? Height, weight, DOB, medication list, list of conditions, procedures, allergies.
This will be the holy grail for anyone and everyone who looks in my chart. This will save me so much time and energy, this will keep me safe.
Next, What’s our main goal? Surgically I mean. I know everyone is focused on the pheo, how it will potentially react during anesthesia. I trust they have that under control. I’ll have an expert team, they’re not new to secreting tumors. What we don’t know is how the MCAS will respond. Mast cells react a lot like pheochromocytomas, in fact most precautions and contraindications are bidirectional. You wake one, you poke the other. This has always been my missing puzzle piece. I worked so hard to get proper care for MCAS, this will be what changes everything. I have to convince them it’s among one of the most important aspects… only one problem: most have never heard of it

They will now.
This is my opportunity to take a well formed document, with simplified research supported information, to make a plan for the complex patients like me. It’s an awareness opportunity of how these conditions interact, and I will be the proof. I know it will work, as long as everyone’s on board…
The first doctor I brought it to was my surgeon. I was thinking it a quick glance and told to give it to the anesthesiologist. Which would make sense, and I was fully prepared to do.
That wasn’t the reaction I received
He flipped through again and again, interested, impressed, he validated my hard work. He told me to make several copies to give to everyone.
I knew in that moment it was going to work out. The relief I felt, well it was profound. Years of trial and tribulation led to this, and it was well received.

Next, I have to meet with the head of my care in order for him to insert his orders for the protocol.
My goal was to have him review the parts I created, and have his specific instructions with a signature.
I’d do the same for my immunologist for the MCAS aspect. Review it all, ask if there’s modifications needed, any additional orders, and get a signature.
Easy enough? Right 😅 I mean in theory, yes. It can be easy, but you never know how someone will respond. In my head, everything was riding on this protocol working.
This all had to be done before pre-op. The person I’d communicate this information to for the surgery is the anesthesiologist. Everyone has a part in my safety, but to me… I needed to make it through this surgery without any complications. The anesthesiologist was the key to that success.
Put your reservations aside, you can do this. Everything has worked out so far. Except the getting a rare metastatic thyroid cancer 😅 right, hyper-vigilance makes sense.
I met with the head of my care at the end of the office day. Sometimes you can feel rushed in a doctors appt, but the clinic was closed and he let me have the floor. My self advocacy was not met with annoyance or resistance, it was applauded and encouraged.
I remember him asking, “why doesn’t your protocol include anything about pheos?” I smiled and replied, “I trust you one hundred percent with all things pheo and adrenal insufficiency. You will be on call, and I know it will be fine. I don’t have that same comfort level with MCAS”
He understood my reservations. We had successfully managed the pheos and adrenal insufficiency countless times. MCAS is not recognized by many healthcare professionals, and can often not be taken seriously.
He took out a form that matched mine, but for pheochromocytomas and paragangliomas in a perioperative setting. We were on the same page. Another wave of relief washed over me
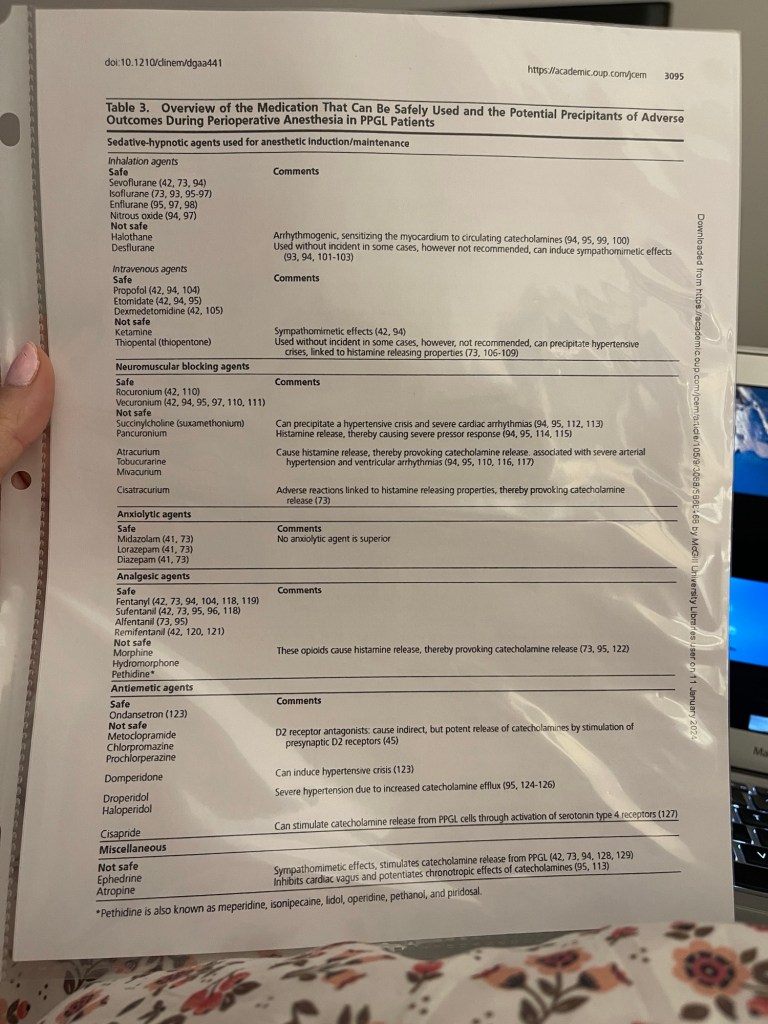
We compared each and every medication to ensure nothing counteracted with one another. There was only one error in my protocol and it referenced a medication that was likely safe for MCAS but is contraindicated with pheos. I was expecting significantly more, but no. One change, that’s it.
I was ecstatic. I left there on top of the world. Not only would he provide his own orders, but he said “we need to be unified in our approach” which would allow for one protocol to be created for all of my conditions.
I know I sound a bit cynical, untrusting, but if you know you know. The number 1 complaint when it comes to rare disease is that doctors don’t communicate to provide unified care. It doesn’t happen often and so it was not lost on me that all throughout this ordeal they had done just that.
I decided to get my hair done in preparation for surgery. Every little bit makes you feel more comfortable, and well – fabulous.
I paused mid hair transformation to consult with my other doctor. It went as well as it could also. Everyone is on the same page and that’s all I hoped for. Time for the real show to begin.

Pre Op…
This is it, this is the day I’ve been preparing for. You’d think I’d be at ease by now, but no. I’m always prepared for any outcome. To fight.
First I had to go do the standard ECG, that went quick. Next, I met with the anesthetist. She informed me although she would not be the one in my surgery, but she would be my voice to communicate everything to the person who is. This would have made me uncomfortable, but she earned my trust. I felt I was in good hands and that it was all going to be okay.
I expressed the goal to everyone that day, to minimize the degranulation of mast cells. We have to keep my body as calm, pain free and safe as possible.
I explained the need for a special bed to reduce pain and expedite healing. I made my request to have my husband able to be with me when waking up in the ICU or PACU. I previously experienced not being able to breathe after having the tube removed upon waking up.
I spoke up for my needs, I was brave.
WE DID IT.
It was all coming together now.
Now, I could breathe. I could allow myself to focus on having the surgery now.
Surgery can’t take my fabulous…
Now that all the logistics were taken care of, I could channel my energy into my FABULOUS! Without it, I wouldn’t be me. So I put on my most fabulous pink and teal lashes, a little thyroid cancer awareness moment. Serge helped me to do my hair, and away we go.

Then THIS happened. My pheo zebra sis Erica showed up all the way from NY to help us through surgery week. What a god send! 🥹
Surgery Day
I woke up with the warmth on my face, the sun was shining for me. This was a good sign. Many people ask me, “how do you cope?” What I can say to that is I’ve spent years mastering the art of focusing on what I can control. There is nothing else for me to control now, and the rest you have to release. Write it down in a journal. Say it to a loved one. Document it in a video. Blog it out.
Affirmations, mantras, meditations, feed your brain things that help you. It can’t harm you to believe everything will be okay.
I don’t remember much of that morning. I just remember the sun.

I remember Serge getting in my twin bed with me, just like we did at my first surgery 13 years ago.

The porter came, it was my time to go. The moment when you’re rolled away, and your person has to say goodbye at the elevator before you’re transported into the OR hallway.
I was ‘parked’ outside the OR I’d be in. My surgeon came to say hi, and ask me how I’m doing. They asked me if I felt mentally strong, and I responded with no doubt, “yes”. The best surgeons will always make you laugh before going in the OR, it lightens the mood and helps you to go in at ease. I showed him my purple drain holders I’d be using, just so they knew the extent of my fabulous.
Next, the anesthesiologist came to my bedside. He told me he’d been studying my protocol and he’d like to go over a few things. We talked about how they’d put in a femoral line after I’m sleeping. How they’d use my existing IV to put me to sleep with propofol in order to avoid degranulation. They’d minimize the use of tourniquets. We talked about anti nausea strategies and the use of a fentanyl pump post op. I was heard.
It’s been a long time since I’ve been in an OR, but this team had my back. The respiratory specialist complimented my lashes, someone held my hand, and before I knew it…
I was waking up in ICU

I’m… awake? Ow, oh no… nauseous.. I’m going to…
“I’m going to throw up”
I didn’t even have my eyes open yet, and there it went. All over my fresh incision. Wonderful. That’s gonna hurt.
Pain, yes, pain, omg, I’m awake. Pain means I’m awake. I did it, I’m here!!!
I AM ALIVE
The surgery was longer than we anticipated, which is also very on brand for me. It was a huge surgery to remove my thyroid with central neck dissection, left neck dissection, and right neck dissection. Serge gave video updates, this was about 5hrs in when they realized the disease was more extensive on the right side than shown.
After I woke up, we got some IV Benadryl going and consistent steroid treatment every 4hrs and I was much better. Almost… weirdly better
I had stayed the in the ICU, and I was cleared to go to the surgical floor. The first day I was up walking, or rather… dancing
They were running my labs continuously, making immediate adjustments to my calcium, vitamin D, magnesium, etc. I felt so.much.better than we anticipated, it was truly a miracle. I am so full of gratitude for the smooth surgical procedure. It was a heck of a time preparing for this point, but it’s an amazing feeling to see how it all came together.
Day 2: post op was more difficult, the swelling and inflammation really hit hard and my breathing was an issue.

But I had an amazing bed bath that evening and it helped with the itchy feeling I had! Highly recommend not waiting until you can take a shower. Have someone do this in bed for the first time, it’s a lot more pleasant and less overwhelming!
Day 3: out of precaution for my breathing difficulties, we did a chest x ray. I’ve had a pulmonary embolism in my previous surgery, so being a higher risk we weren’t taking any chances.

Day 4: The swelling was doing its thing. The drains were uncomfortable. The only thing that helped was small frequent walks, it’s the best medicine.

I got one of my drains removed on this day, and although I was so scared to have it yanked out…. It actually some how felt good. Like a gross mixture of bad and oh so good 😂

I had a really bad breathing night this night. The drain removal alone would have caused a mast cell response. I believe I was transitioned off the pain medicine this day also. We have to expect some kinks and make adjustments as it happens.
Day 5: We began talking about discharge. I had the other 2 drains removed. I had my first real shower. Definitely overdid it again 😂 classic.

I began having another choking episode. My body was letting me know to slow it down a little, be cautious, and stay on top of the protocol. This was the night I found out if I’d had an anaphylactoid crisis, they would not be able to respond immediately. They could only give me the prescribed meds that were every 4-6hrs.
I always bring my own medications to the hospital, my own steroid injection for crisis, and every other form of medicine I need because of situations like this. However it was really eye opening to hear they’d have to call a code if I couldn’t breathe because of the way it was written. My protocol will be updated to reflect the need for AS NEEDED solucortef injection + Benadryl. Please ensure when you’re hospitalized that any emergency protocols are properly prescribed.
Day 6: DISCHARGE DAY! I honestly never thought it’d be possible to be discharged so quickly. It was a tough transition, but I was happy to be out of the hospital. We stayed close by at an air b&b to ensure we had close access.

To continue reading about my experience with thyroid cancer and post op info, follow along as the story unfolds.
You can also follow me on Instagram to keep up with the daily pheo vs fabulous adventures